AL-FATIHAH
*************************
 *************************
*************************
Ostreoarthritis
What Is Ostreoarthritis / OA? |
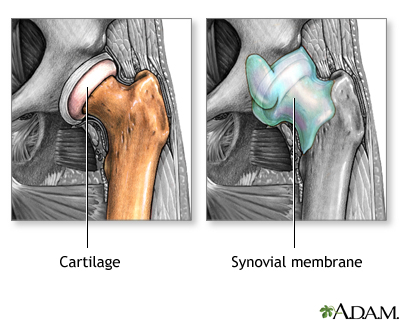
When you feel stiff and achy and your joints hurt, there's a good chance you have osteoarthritis or OA, one of the oldest and most common forms of arthritis. Often known as the "wear and tear" kind of arthritis, osteoarthritis is a chronic condition characterized by the breakdown of the joint's cartilage. Because cartilage is the part of the joint that cushions the ends of the bones and allows the joint to move easily, when it breaks down, bones rub against each other, causing stiffness, pain and even loss of movement. Osteoarthritis dates back to the Ice Age and now some 27 million Americans live with it. But even after all those years, there is no cure and no definitive cause has been discovered. Contributing factors, however, may include age, obesity, injury, overuse and genetics. Knowing and controlling these risk factors can help you minimize your risk or avoid getting osteoarthritis altogether. There are several stages of osteoarthritis:
Changes in the cartilage and bones of your joints can lead to pain, stiffness and even limitations in how you can use your body.
Deterioration of cartilage can:
You may hear osteoarthritis referred to by many different names including degenerative joint disease, osteoarthrosis, hypertrophic arthritis and degenerative arthritis. But whatever it's called, osteoarthritis can be a manageable part of your life when you're armed with resources to keep it under control. What Causes OA? There isn't one main cause of osteoarthritis, but there are several risk factors that can make you more likely to develop it. Knowing those risks and doing what you can to fight them can actually help lower your chances of ending up with the disease. There are two types of osteoarthritis – primary and secondary. Primary osteoarthritis is related to aging and the "wear and tear" of life. The older you are, the more likely you are to have some degree of primary arthritis. Secondary osteoarthritis is attributed to some more specific known cause such as injury or obesity. These are the most common risk factors that can work together to cause osteoarthritis.
Who Is At Risk?Osteoarthritis doesn't discriminate. It is common in all races and backgrounds. In fact, it is the most common type of arthritis in the United States, with nearly 27 million people affected by it. Osteoarthritis of the knee and hips is the most common cause of arthritis-related disability in the U.S. The older you are, the greater your risk for osteoarthritis. It most commonly affects middle-aged and older people, with most people getting it after age 45. Osteoarthritis affects both men and women. However, overall, women are more affected than men, especially with osteoarthritis of the fingers and the knees. Men under age 55 are more likely to have osteoarthritis than women of the same age. After age 55, women are more commonly affected. Researchers believe that because women have broader hips than men, this puts more long-term stress on the knees which means more osteoarthritis. In a 2008 study which suggested that nearly 1 in 2 people will develop knee osteoarthritis before they turn 85, researchers found that the risk rose to 2 in 3 for people who were overweight or obese. Although race and sex seemed to have no effect on the risk of getting knee osteoarthritis, the study found that the chances went up significantly with increasing body weight. Those who stayed at a normal weight throughout their lives had the lowest lifetime risk of any group in the study – 30 percent. Those whose weight fluctuated from normal to overweight/obese had the highest lifetime risk of knee osteoarthritis – 60 percent.
What Are The Symptoms? Every person, of course, is different, so every person may be affected differently by osteoarthritis. But there are general symptoms to look for if you suspect you may have osteoarthritis. Osteoarthritis most commonly occurs in the weight-bearing joints of the hips, knees and lower back. It also affects the neck, small finger joints, the base of the thumb and the big toe. Osteoarthritis rarely affects other joints except when injury or stress is involved. Most often, osteoarthritis develops gradually. It may start out as soreness or stiffness that is more of a nuisance than a medical issue. Your pain may be moderate, occasional and may not interfere with your day-to-day activities. Some people's osteoarthritis will never progress past this early stage. For some people, however, their osteoarthritis will advance to a point where it interferes with everyday life. Pain and stiffness could make it difficult for them to walk, climb stairs or sleep. Rarely, a person with osteoarthritis will experience sudden signs of inflammation such as redness, pain and swelling known as inflammatory or erosive osteoarthritis. The most common signs and symptoms of osteoarthritis are:
 If osteoarthritis is in the hips, you may experience:
 If osteoarthritis is in the knees, you may experience:
 If osteoarthritis is in the fingers, you may experience:
 If osteoarthritis is in the feet, you may experience:
If osteoarthritis is in the spine, you may experience:
It is important that you take an active role in the treatment of your osteoarthritis and in the prevention of additional joint damage. There are even steps you can take to lower your risk for developing osteoarthritis at all. However, it is crucial that you go to your doctor for a diagnosis before you treat osteoarthritis on your own. Several other conditions seem similar to osteoarthritis, but are treated in different ways. Once you get a proper diagnosis, you can begin early, aggressive action. Treatment may change as the disease progresses or improves so it's important that you continue to play an active part in your osteoarthritis management. How Is OA Diagnosed? Early diagnosis and treatment is the key to controlling osteoarthritis. Your doctor will take a medical history and perform a physical exam to assess your disease activity. He or she may use X-rays to confirm or strengthen a diagnosis, although most people over 60 reflect osteoarthritis on X-ray while only one-third have actual symptoms. Osteoarthritis is mostly common diagnosed by a family physician, but often a patient may later be referred to an arthritis specialist, called a rheumatologist, for specific treatment. Other health professionals you may encounter along the way may include orthopaedic surgeons, physical therapists and occupational therapists. Your doctor will use four main tools to determine your diagnosis: your medical history, a physical exam, X-rays, and joint aspiration. The medical history and physical exam will be what he or she bases the diagnosis on, using tests such as X-rays and joint aspirations to confirm the diagnosis. Medical History A medical history probably is your doctor's best tool for diagnosing osteoarthritis. The more your doctor knows about you, the faster and better he will be able to diagnose your condition and determine the best treatment for you. Your doctor will want to know about your health background, including any diseases or conditions you currently have, any allergies you have to medications or other substances, and surgeries and other medical procedures you've been through. Following is a list of questions your doctor might ask:
During your medical history, your doctor will want you to describe any pain you are experiencing. Since pain is the number one complaint of people with osteoarthritis, it is important for you to describe your pain accurately. Is it burning, grinding, sharp or achy? When do you normally notice your pain and other symptoms? Are they tied to an activity or lack of activity? Are your symptoms, including pain, constant, or do they come and go? Have they gotten better, worse or stayed the same throughout time? If your pain increases during the day or becomes worse in the evening, you may have osteoarthritis. This is a lot of information to remember. It is a good idea to write down some answers to these questions before you visit the doctor. Physical Exam Your doctor also will perform a physical exam to determine a diagnosis. He will be looking for common symptoms reported in osteoarthritis, including:
You may be asked to stand so your doctor can determine how your range-of-motion and mobility have been affected. Lab Tests Your doctor will probably use lab tests to confirm a diagnosis of osteoarthritis.
Because there is no surefire test that diagnosis osteoarthritis, your doctor will use your medical history, physical exam and lab test results to look for indicators of osteoarthritis, including:
Make sure you get the proper information about your diagnosis from your doctor before you leave the office. This includes basic information about your condition and its management. Be sure to ask the following:
How Is OA Treated? There is no cure for osteoarthritis, but there are a number of treatments, therapies and exercises that can help with the symptoms. Osteoarthritis drugs Painkillers (analgesics) often help the symptoms although they don't affect the arthritis itself. They are best used occasionally for bad spells, or when extra exercise is likely. Paracetamol is usually the best painkiller to try first. Combined painkillers (e.g. cocodamol, codydramol) contain paracetamol and a second codeine-like drug and may be helpful for more severe pain. 1- Non-steroidal anti-inflammatory drugs may be prescribed if inflammation in the joint is contributing to the pain and stiffness. A low dose of ibuprofen or naproxen are common options. These will usually be given with a tablet to help protect the stomach. 2- NSAID creams, gels or liquids to rub on often help, especially for knee and hand osteoarthritis. These can be helpful if you have trouble taking tablets. 3- Capsaicin cream (made from capsicum, the pepper plant) is also an effective painkiller. It needs to be regularly applied each day to be effective. 4- Stronger painkillers (e.g. tramadol, nefopam, meptazinol) may be required for people with severe pain if other medications don't provide adequate relief. Some opioids can be given as a plaster patch on the skin which can give pain relief for a number of days. Because these tablets and creams work in different ways it may be useful to combine them. Your chemist can advise you and offer paracetamol, and some low-dose NSAID tablets and creams without a prescription. However, you can only get capsaicin cream, most NSAID tablets and creams, strong combined painkillers and opioids on prescription from your doctor. 5- Injections are sometimes given directly into the affected joint: - A steroid injection into the joint may improve pain for several weeks or even months, especially in a hip, knee or thumb. This is mainly reserved for very painful osteoarthritis. - An injection of hyaluronan into the knee may help a few people with knee osteoarthritis, although it is not often used. Hyaluronan is similar to the thick, viscous component of normal joint fluid and is normally given as a course of injections once a week for 3–5 weeks, or occasionally as a single injection. Physical Therapies Physiotherapy can play an important part in keeping the joints mobile. A physiotherapist or can devise a programme of exercises tailored to your individual needs. An occupational therapist will be able to advise on techniques, aids and appliances that will allow you to get on with your daily jobs without putting too much strain on your joints. Surgery Surgery may be recommended if pain is very severe and/or you have mobility problems. Hip and knee replacements can give substantial pain relief in cases where other treatments haven't helped. Sometimes, if your knee locks, keyhole surgery techniques may be used to wash out loose fragments of bone and other tissue from the joint (this is called arthroscopic lavage and isn't recommended unless the knee locks). Additional procedures are occasionally carried out – such as smoothing the surfaces of the joint and trimming torn soft cartilage (this is called debridement). These techniques can't repair the damage to the knee but may offer pain relief in the earlier stages of osteoarthritis. Complementary Therapies
Complementary and alternative medicine refers to a wide range of therapies and practices which are outside the mainstream of medicine.If you use complementary and alternative medicine, it is important that you discuss this with your doctor and health care team and don’t suddenly stop your conventional medicine. You should be suspicious of any complementary and alternative medicine practitioner who advises you to do so.Osteopaths and chiropractors are legally recognized professionals just like doctors, nurses and physiotherapists.
Watch Your Diet And Eat For Your Health What one eats affects the entire body. Foods contain so much more than vitamins, minerals, fats, carbohydrates and protein. Holistic nutrition approaches pain relief from arthritis by suggesting arthritis patients avoid certain foods that can exacerbate the inflammatory response. Chemicals within certain foods can increase inflammation or reduce inflammation.
Foods Behind Popular Healing TrendsThese byproducts are the subject of intense debate in the medical world and praise from the holistic healing and alternative medicine communities for their supposed powers over bacteria, infection, pain, and disease. While speculation continues as to the extent and nature of their healing capabilities, many users attribute their relief or recovery to the unique properties of one or more of these substances. From noni juice, Olive oil, Rose Hips and coconut oil to apple cider vinegar and raw honey, natural products are subject to trends and fads within the organic and holistic healing communities. The healing properties they supposedly possess, however, inspire both believers and skeptics to experiment with their curative powers. Noni JuiceDerived from a tropical island fruit that resembles a cross between a kiwi and a potato in appearance, the noni fruit possesses a foul taste but a powerful healing agent within its substance, according to its holistic researchers. The bottled juice is a popular choice at health food emporiums and alternative medicine venues. Hailed for its pain-relieving properties, noni is a particularly popular choice for chronic pain sufferers, including unconfirmed fibromyalgia patients, arthritis sufferers, and chronic muscle pain sufferers. The juice is also used as a health supplement in diet and as a deterrent to certain diseases and conditions. Virgin conut OilAlternative medicine followers and natural dietitians promote virgin or natural coconut oil as a virtual miracle substance. The lightly-flavored oil solidifies in cool temperatures, forming a paste that many users melt and mix with coffee to consume or spread across toast as a butter substitute. Olive oil and Rose hips are another two elements that contain essential oil which is proven good for preventing osteoarthritis. Omega-3 Fatty acids Above all, it's been suggested that, increasing the amount of essential fatty acids in your diet, particularly omega-3 fatty acids found in oily fish, should help reduce the risk of osteoarthritis. 
 |
Komen Tentang Blog Ini:




 Warm up lah dulu...
Warm up lah dulu...
 Yeaah...Gerak kiri/kanan cam nak bersilat...
Yeaah...Gerak kiri/kanan cam nak bersilat...
 Pusing bahu n Lenggang kiri/kanan...
Pusing bahu n Lenggang kiri/kanan... Bongkok n Pusing kepala..!
Bongkok n Pusing kepala..!

 Lor... Ko amik gambo ker..?
Lor... Ko amik gambo ker..? Adehh... Sakit pinggang la plak..!
Adehh... Sakit pinggang la plak..! Hahaha.... Pasal tak leh stop ni...?
Hahaha.... Pasal tak leh stop ni...? *The tale 0f you and I*
you gave walking sticks to others
yet you yourself were limping
you offered a lending hand
but it was you who needed help
you wore shields and armours
but it wasnt the outside that needed protection
you claimed others as foes and threats
yet you stabbed your very own heart
you blamed the time for being envious
was it not you who made the clock?
you walked the road with glitters and jewels
but back in home you slept on dirt
you conquered the lands and the oceans and skies
yet you moaned and screamed in dreams
you were the king of glorious men
but you were held captive of unseen strings
you claimed yourself a proud free man
yet you were chained to your old ventriloquist>
"By the power of Truth...."

























Post a Comment